Drug addiction treatment, also known as substance use disorder (SUD) treatment, encompasses a range of evidence-based approaches to help individuals overcome dependence on substances like alcohol, opioids, stimulants, and others.
Addiction is a chronic brain disease involving compulsive drug-seeking despite harm, but recovery is possible with proper intervention. Effective treatment addresses physical dependence, psychological factors, and social issues, often combining medications, therapy, and support. Success rates vary (relapse 40–60%, similar to other chronic diseases), but integrated care improves outcomes significantly.
Understanding Addiction and Treatment Principles
Addiction alters brain reward circuits, making quitting difficult. Treatment principles (NIDA/SAMHSA):
- No single approach fits all.
- Effective programs address multiple needs.
- Treatment duration matters (minimum 3 months).
- Medications + behavioral therapies are ideal.
- Continuous monitoring prevents relapse.
Levels of care: Detox, inpatient/residential, outpatient/intensive outpatient (IOP), sober living.
Key Treatment Approaches
Medication-Assisted Treatment (MAT)
MAT combines FDA-approved medications with counseling. Gold standard for opioids/alcohol; reduces cravings/overdose risk.
- Opioids: Methadone, buprenorphine, naltrexone.
- Alcohol: Naltrexone, acamprosate, disulfiram.
Behavioral Therapies
Core of treatment; modify attitudes/behaviors.
- Cognitive Behavioral Therapy (CBT): Identifies triggers, builds coping skills.
- Contingency Management: Rewards abstinence.
- Motivational Interviewing: Enhances motivation.
- 12-Step Facilitation: Supports AA/NA involvement.
Group/individual sessions common.
Support Groups
Peer-led like AA/NA; provide community/accountability.
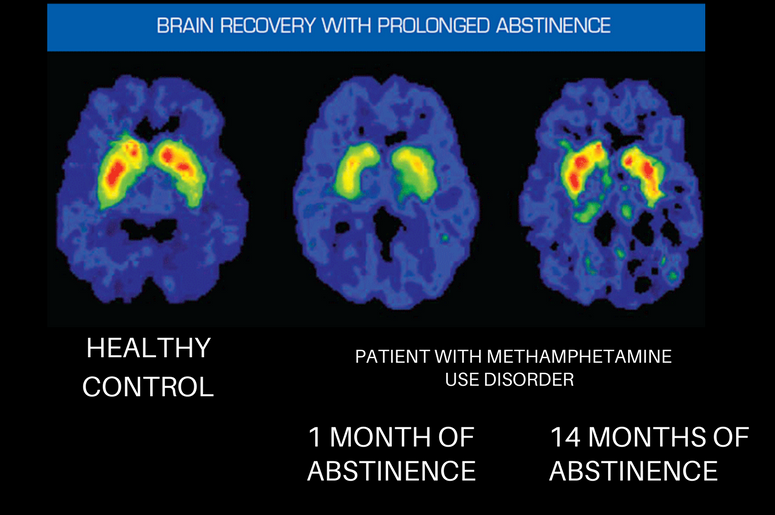
Neuroscience of Recovery
Addiction changes brain structure/function; recovery shows neuroplasticity with abstinence/therapy.
Current Statistics and Effectiveness
~22–29 million U.S. adults in recovery (2023–2024 data). Relapse rates 40–60%; treatment completion ~42%. MAT halves overdose risk. Longer treatment (>90 days) boosts success.
Emerging Developments in 2025
- Personalized/genetic-guided MAT.
- Telehealth/digital apps.
- Holistic/trauma-informed care.
- Psychedelics (ketamine/psilocybin trials).
- AI monitoring, brain stimulation.
Treatment evolves toward integrated, personalized care. Recovery is achievable—seek professional help via SAMHSA helpline or providers.
More articles by ZMR Researche:
https://www.zionmarketresearch.com/de/report/birch-water-market
https://www.zionmarketresearch.com/de/report/cell-roller-bottles-market
https://www.zionmarketresearch.com/de/report/cheese-liners-market
https://www.zionmarketresearch.com/de/report/technical-consumer-goods-tcg-market
https://www.zionmarketresearch.com/de/report/sous-vide-machine-market